Stress Incontinence Of Urine
Medically Reviewed By Dr. Jessica Lubahn, Urologist and Founder of ONDRwear
Stress incontinence of urine is the uncontrolled leakage of urine. Stress incontinence can happen after childbirth, and it is much more common as a person ages. After age 65, 1 in every 2 women may find themselves with unwanted bladder leakage periodically. Besides the physical toll, this condition can also impact women emotionally. Women find themselves afraid to participate in normal activities or on a constant hunt for the toilet.
What Causes Bladder Leakage?
Bladder leakage itself is not a disease, but rather a symptom of other underlying conditions. There are several forms of incontinence. One of the most common is stress incontinence. Stress incontinence of urine is caused by weak or damaged pelvic floor or sphincter muscles. The chronic conditions listed below can lead to damaged pelvic floor muscles.
Pelvic Floor Dysfunction Causes:
- Constipation
- Organ prolapse
- Pregnancy
- Hormonal changes such as menopause
- Low back injury
- Pelvic trauma or injury
- Obesity
- Heavy athletic training
Understanding Pelvic Floor Anatomy
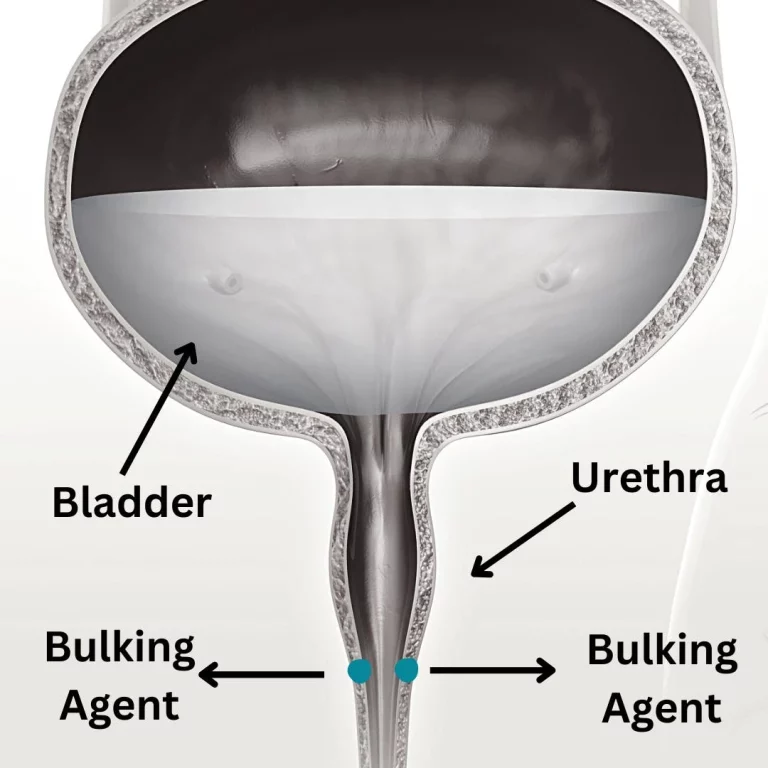
The pelvic floor refers to a grouping of muscles that are attached to your pelvis and form the base of your core. These muscles have a variety of roles, one of which includes bladder control. Your pelvic muscles surround your bladder and urethra (the tube that is responsible for carrying urine out of your body) and help to maintain the control of urine as you pee.
If your pelvic muscles have been weakened or stretched, you may find yourself leaking pee when exercising or any other physical activity that puts pressure on the bladder. Common triggers include sneezing, coughing, laughing, lifting, bending. The leakage may be as mild as a few drops to as severe as several tablespoons (1).
Treatments For Stress Incontinence: How To Stop A Leaking Bladder
1. Make Lifestyle Changes
Just because you have this issue, does not mean there is nothing that can be done. Here are some immediate changes that can improve your situation.
- Use absorbent pads or underwear
- Smoking cessation
- Avoid constipation by methods like drinking more water, eating plenty of fiber, and being more active.
- Use moisturizing creams, lotions, barrier creams that can help protect your skin from leaking urine.
2. Pelvic Floor Physical Therapy
Getting help from a pelvic floor physical therapist can be of great benefit. Pelvic floor muscle exercises can help many people. Kegel exercises are a great place to start when you’re trying to put an end to leaking pee!
Kegel exercises can be done pretty much anywhere and help strengthen the muscles of your:
- Bladder
- Pelvic floor
- Uterus
- Small intestines; and
- Rectum
A visit to a pelvic floor physical therapist may be even more effective. Specially trained in pelvic floor dysfunction, pelvic floor physical therapists can give you a professional assessment to determine the exact cause of your pelvic issues (2).
They can then create an individualized plan for you that may include things such as:
- Specific exercises to help you strengthen your pelvic floor
- Dietary changes, including foods you may want to avoid when dealing with urinary incontinence
3. Weight Loss
A 2010 study found that losing weight can help to reduce the incidence of stress urinary incontinence episodes. Since losing extra body weight removes some pressure on the bladder and pelvic floor, it can help decrease urinary incontinence (3).
Related: Is My Vagina Normal? Plus A Female Anatomy Chart
4. Exercise For Incontinence? Yes!
It may be counterintuitive to exercise more when you are leaking pee with exercise, but maintaining a regular exercise routine can help strengthen your pelvic muscles.
You will want the focus of your exercise to be on strengthening your pelvic floor, so instead of high-impact workouts like aerobics, CrossFit, or jogging, try exercises that strengthen your core, such as Pilates. Core exercises can help to put an end to leaking pee when exercising (3).
5. Use A Vaginal Pessary
A vaginal pessary is a pliable, removable device that is placed into the vagina to help support areas of pelvic organ prolapse (POP). POP results when the bladder, uterus, or rectum drops or bulges down towards a woman’s vagina (4).
Typically made of silicone, pessaries come in a variety of types, including:
- Ring: A circular device that may be easily inserted and removed without the help of a doctor. There may be a bump on this to help support the urethra against incontinence.
- Gelhorn: A disc-shaped device with a small knob in the center. A Gelhorn pessary is used for severe prolapse.
- Gehrung: This U-shaped device is molded to fit the individual and is used for more advanced uterine prolapse.
Over the counter, disposable vaginal suppository options are also available. Your doctor will be able to help determine the type of pessary that will be the best option for you to prevent peeing when exercising.
6. Bladder Training
Bladder training is a common way to manage urinary incontinence and put an end to peeing when exercising.
A pelvic floor physical therapist or pelvic pain doctor can help with this option and may recommend methods such as:
- Delaying urination
This method may start by trying to hold your urine for 5 minutes. You will then gradually increase the time until you are urinating every 3 to 4 hours. - Scheduling bathroom trips
You may be encouraged to go to the bathroom at specific times, whether you feel the urge to pee or not. For instance, you may start by going to the bathroom hourly and then gradually increase the time until you find the schedule that works most comfortably for your bladder.
Bladder training can help by:
- Increasing the amount of pee your bladder can hold
- Lengthening the amount of time between trips to the bathroom
- Improving your control over the urge to urinate
7. Consider Surgery
In case of severe stress incontinence, surgery may be required. Most surgeries for bladder incontinence fall into the following categories:
- Urethral bulking agents
- Sling procedures
- Bladder neck suspension procedures
As with any surgery, incontinence surgery comes with a list of risks, including:
- Urinary tract infection (UTI)
- Temporary difficulty in urination
- Urinary retention (incomplete emptying of the bladder)
- The development of an overactive bladder
- Difficult or painful intercourse
Due to its invasive nature, surgery is usually done as a last resort.
Sources:
- https://pubmed.ncbi.nlm.nih.gov/25078140/
- https://www.niddk.nih.gov/health-information/urologic-diseases/kegel-exercises?dkrd=/health-information/urologic-diseases/bladder-control-problems-women/kegel-exercises
- https://pubmed.ncbi.nlm.nih.gov/20643425/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909791/
We discuss products we think are useful to people. If you buy something through our links, we may earn a commission. Remember to check with your personal physician to see if a product recommended is right for you.