- All Articles
- Gynecology
- Fertility
- Pregnancy
- Breast Health
- Skin
- Hormones
- Mental Health
- Cardiology
- Pelvic Dysfunction
- Pediatrics
- General Health
- Postpartum
- Lifestyle
Snoring And Menopause Hormones: Is It Sleep Apnea?
If you’re wondering about snoring and menopause, you’re not alone....
Read MorePostpartum Diet Plan: Tips For Healthy Weight Loss
The postpartum period is a critical phase in a new...
Read MorePainful Periods With PCOS: Causes And Treatment
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that...
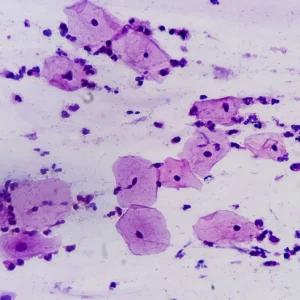
Read MoreDoes A Pap Smear Test For Gonorrhea?
A Pap smear test, also known as a Pap test,...
Read MoreDoes A Pap Smear Hurt? What To Do Before The Test
Many women wonder, “Does a Pap smear hurt?” The good...
Read MoreHow To Prepare For A Pap Smear: Cancer Screening Test
Many people wonder if they need to prepare for a...
Read MoreCan A Pap Smear Detect STD Sexually Transmitted Disease
Medically reviewed by Dr. Shieva Ghofrany A Pap smear, also...
Read MoreAppendicitis Vs Ovarian Cyst
There are some differences between the symptoms of ovarian cysts...
Read MoreIs Slugging Good For Acne-Prone Skin? Derm Explains
Many patients wonder, Can Slugging Help Acne? Board-certified Dermatologist and...
Read MoreWhy Do I Pee When I Sneeze Female: Stress Incontinence Of Urine
Experiencing an involuntary loss of urine while sneezing is a...
Read MoreDoctor Explains Treatment For Postpartum Foot Pain
Postpartum foot pain is a common issue. It is experienced...
Read MoreJuvederm Vs Botox: Dermatologist Explains
When it comes to the appearance of wrinkles, there are...
Read MoreDoes A Pap Smear Test For Gonorrhea?
A Pap smear test, also known as a Pap test,...
Read MoreDoes A Pap Smear Hurt? What To Do Before The Test
Many women wonder, “Does a Pap smear hurt?” The good...
Read MoreHow To Prepare For A Pap Smear: Cancer Screening Test
Many people wonder if they need to prepare for a...
Read MoreCan A Pap Smear Detect STD Sexually Transmitted Disease
Medically reviewed by Dr. Shieva Ghofrany A Pap smear, also...
Read MoreCan You Catch HPV From A Toilet Seat?
HPV is referred to as the human papillomavirus; it is a...
Read MoreVaginal Atrophy Treatment: Different Remedies You Can Try
Vaginal atrophy, known as atrophic vaginitis, refers to the drying,...
Read MoreWhat is Vaginismus – and Why Does it Occur?
What is Vaginismus? Vaginismus occurs due to the spasm or...
Read MoreWhat is Dyspareunia: Causes, Symptoms, and Treatments
What is Dyspareunia? Dyspareunia is the recurring genital or pelvic...
Read MoreIUDs For Birth Control: 10 Questions Answered By An Expert Doctor
What Is An IUD? IUD stands for “intrauterine device”. It...
Read MoreSleep and Weight Loss
Relationship between Sleep and Weight Loss Losing weight isn’t just...
Read MoreWhat is Libido? A Quick Review
What is Libido? The term “Libido” simply means the desire...
Read MoreFemale Orgasm: 3 Myths Debunked by an ObGyn
Female Orgasm Facts Amongst friends, the conversation about sex always...
Read MoreHow to know if you have PCOS or Polycystic Ovarian Syndrome?
PCOS is also known as Polycystic Ovarian Syndrome. It is...
Read More5 Questions to ask Fertility Doctor
Social media, the internet, and even friends and family may...
Read More5 Online Fertility Calculators You Can Use Today
If you’re trying to conceive, then one of the things...
Read MoreAdenomyosis And Fertility
It is controversial whether adenomyosis and infertility are linked because...
Read MorePeak Ovulation: 5 Ways to Track Ovulation Effectively
If you are trying to conceive, tracking your peak ovulation period is...
Read MoreDischarge Changes When You Ovulate: What to Know
A woman’s body produces many fluids (that are totally normal),...
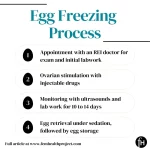
Read MoreDoes Insurance Cover Egg Freezing?
If you think you might want to delay pregnancy and...
Read MoreDealing with Infertility and Infertility Depression – The Impact of Infertility on Mental Health
Infertility Depression The word ‘infertility,’ often brings to mind doctor’s...
Read MorePGT Testing: What Is Preimplantation Genetic Testing In IVF?
Preimplantation genetic testing (PGT) is a way for people planning...
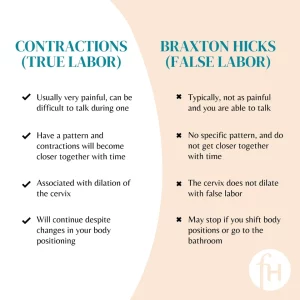
Read MoreBraxton Hicks Vs. Contractions In Real Labor
Braxton Hicks contractions happen in almost all pregnancies, but some...
Read MoreDry Mouth During Pregnancy: Symptoms, Causes, & Treatment
Dry mouth during pregnancy is almost always normal. It occurs...
Read MoreBirth Control Pills vs. IUD: Choosing The Right Method
Choosing a birth control method often seems like a difficult...
Read MoreWhat Is an Ectopic Pregnancy?
Ectopic Pregnancy Stories Normally, pregnancy occurs when a fertilized egg...
Read MoreTdap Vaccine For Pregnancy: Should You Get The TDAP Vaccine During Pregnancy?
First, What Is The TDap Vaccine? The Tdap vaccine provides...
Read MoreConstipation During Pregnancy
Can Pregnancy Cause Constipation? Yes! Unfortunately, pregnancy and constipation often...
Read MoreCost For Cord Blood Banking
Cord blood banking is something to consider if you are...
Read MoreSpotting in Pregnancy
While spotting is a relative common occurrence in early pregnancy,...
Read MoreInsomnia In Pregnancy
Insomnia in pregnancy is very common. Studies estimate that anywhere...
Read MoreLife or Death: On Being Pregnant and Black
In 2018, tennis star Serena Williams, while recovering in the...
Read MoreHow Early Can You Take a Pregnancy Test? The Real Answers Here!
One of the most anxious moments women go through is...
Read MoreBreast Lump Pregnancy – Should you worry?
Finding a breast lump in pregnancy can be very scary,...
Read MoreBreast Milk Color – Can Breast Milk Be Different Colors?
Breast milk color is often thought to be white. So,...
Read MoreWhat is Breastfeeding Let Down and is it Bad?
Breastfeeding Let Down In terms of breastfeeding, “let down” is...
Read MoreFibroadenoma On Breast
A breast fibroadenoma is not cancer. It is a breast lump that...
Read MoreDoes A Mammogram Hurt?
A mammogram for breast cancer screening may hurt in some...
Read MoreWhat You Should Know About Tuberous Breasts
Tuberous breasts, also known as tubular breasts or breast hypoplasia, are a...
Read MoreSymptoms Of Breast Cancer
Breast cancer symptoms can be different for different people. Some...
Read MoreWhat to Expect From a 3D Mammogram
Are you wondering what to expect from a 3D mammogram?...
Read More8 Scientific Breastfeeding Benefits
If you are newly pregnant or approaching your due date,...
Read MoreIs Slugging Good For Acne-Prone Skin? Derm Explains
Many patients wonder, Can Slugging Help Acne? Board-certified Dermatologist and...
Read MoreJuvederm Vs Botox: Dermatologist Explains
When it comes to the appearance of wrinkles, there are...
Read MoreWhat Causes Dark Circles Under Eyes? What to Watch Out For!
There are common and various reasons why dark circles develop,...
Read MoreDry Hair: Causes and Treatments
Dry hair affects both men and women and can happen...
Read MoreHow do Retinoids help my Skin?
What are retinoids? Retinoids are a class of medications derived...
Read MoreSkin Care: How Long for Scars to Fade
Tumbling off a bike, surgery, acne, or burn will all...
Read MoreSkin Elasticity: Reducing the Onset of Elastosis
The human skin has an elastic quality to it. This skin...
Read MoreWhat are stretch marks?
Stretch marks are lines that appear on the skin in parallel...
Read MoreFoods that Cause Acne – According to Dermatologists
Acne vulgaris is a very common dermatologic condition that affects...
Read MoreHow To Deal With Hair Loss From Stress
Many people wonder if their hair loss is related to...
Read MorePainful Periods With PCOS: Causes And Treatment
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that...
Read MoreSigns Of Early Menopause
One of the earliest signs of menopause is irregular bleeding...
Read MoreIs PCOS Treatable?
Polycystic Ovary Syndrome, abbreviated as PCOS, is the most common...
Read MoreThyroid Eye Bulging And More Thyroid Eye Disease Symptoms
Thyroid eye disease is a condition that occurs in nearly...
Read MoreAt What Age Is Menopause Going To Happen To Me?
Many people wonder about what age menopause will occur. Menopause...
Read MoreThyroid Diet And Nutrition
What Food Should I Avoid If I Have Thyroid Problems?...
Read MoreSymptoms Of An Overactive Thyroid (Hyperthyroidism Symptoms)
Hyperthyroidism, also known as “overactive thyroid”, is a condition where...
Read MoreIs PCOS An Autoimmune Disease
Many people wonder, “Is PCOS A Autoimmune Disease?” The answer?...
Read MorePerimenopause Sex Drive: Libido Decrease Or Increase?
Many women have questions and concerns surrounding their perimenopause sex...
Read MoreUnderstanding Dexamethasone Suppression Tests
There are 3 types of dexamethasone suppression tests. The low-dose...
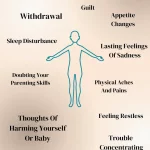
Read MoreSymptoms For Postpartum Depression
It is critical that women and pregnant persons are supported mentally, physically,...
Read MoreWhat Is Gaslighting And What You Can Do About It
Gaslighting is a form of emotional abuse where the victim starts to...
Read MoreBaby Blues Syndrome Vs Postpartum Depression
The days and months after giving birth can be a psychologically challenging...
Read MoreGaslighting In A Relationship
Is Gaslighting Abusive? Yes. Gaslighting is a type of psychological abuse where...
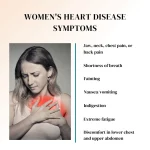
Read MoreWomen Heart Disease Symptoms
Heart disease is a catch-all term for several heart conditions...
Read MoreIs Red Wine Good For You? A Cardiologist Explains The Link Between Red Wine And Heart Disease.
Is red wine good for my heart…or not? From wellness...
Read MoreWhy Do I Pee When I Sneeze Female: Stress Incontinence Of Urine
Experiencing an involuntary loss of urine while sneezing is a...
Read MoreStress Incontinence Of Urine
Medically Reviewed By Dr. Jessica Lubahn, Urologist and Founder of...
Read MoreTreatment For Pelvic Floor Muscle Disorders & Dysfunction
Pelvic Floor Muscles & Anatomy The pelvic floor muscles are...
Read MoreDisposable Underwear For Incontinence & Postpartum
When it comes to incontinence or vaginal bleeding, disposable underwear...
Read MoreUrethral Bulking Agents For Urinary Incontinence
Urethral bulking injections are used to treat stress urinary incontinence,...
Read MoreHow To Heal Perineal Scar Tissue After Childbirth
Perineum scar tissue is a common issue that many women...
Read MoreWhen to Start Cow’s Milk for Baby: Making the Switch
If you are considering making the switch to cow’s milk...
Read More5 Sleep-Training Methods For Babies You Can Follow
As new parents, it may be difficult adjusting to your...
Read MoreWhen to Start Sippy Cup: The Best Time for Your Baby
Are you unsure about when you should introduce the sippy...
Read MoreWhen Do Babies Start Laughing? The Developmental Stages to Know
As your little one begins to grow and achieve milestones,...
Read More5 Signs of Postpartum Depression to Watch Out For
About 10% of moms who have just given birth experience...
Read MoreWhat Are The Benefits Of Infant Massage?
Infant massage is a process of gently rubbing the muscles...
Read MoreWhat Are Baby Sleep Regressions? What to Know and How to Handle Them
Is your little one waking up every 20 minutes and...
Read MoreFeeding For Newborn: How Much? How Often?
Feeding newborns can seem like a daunting task. Remember that...
Read MoreBest Teether For Molars In Baby?
Teething hurts! Every parent needs to have a great teether...
Read MoreWhen To Stop Swaddling Your Newborn
Many parents use a swaddle in the early days of...
Read MoreBest Montessori Toys For 3 Year Olds
Montessori learning is a very popular way to have your...
Read MoreAppendicitis Vs Ovarian Cyst
There are some differences between the symptoms of ovarian cysts...
Read MoreIs Dry Shampoo Safe? Potential Damage & Usage Recommendations
Dry shampoo is a product designed to freshen hair between...
Read MorePreventing Eye Injuries in Children: Advice from a Cornea Specialist
Our most prized possession (okay maybe I’m a bit biased),...
Read MoreAllergic To Peaches: Symptoms, Causes, And Treatment
Peaches are a sweet and delicious fruit enjoyed by many...
Read MoreBladder Control by Age: What to Expect
If you’ve noticed a change in your ability to hold...
Read MoreMy voice is hoarse! How do I keep my voice healthy?
Authors: Dr. Anju Patel, Shielah Mauntana Medically reviewed by ENT...
Read MoreSinus Headache vs. Migraine: Identification and Treatment
The most common headache is a tension headache that usually...
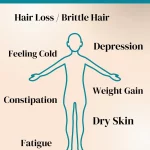
Read MoreSymptoms For Underactive Thyroid (Hypothyroidism)
Our hypothyroidism symptoms checklist below will help you with knowing the signs...
Read MoreCovid-19 Vaccine: Eliminating Misinformation
Despite evidence showing the effectiveness of the Covid-19 vaccine at...
Read MoreWhat Cholesterol Is Good?
Cholesterol is an important organic molecule that is essential to...
Read MoreSustainable Underwear Brands
Looking to live that sustainable life? With the fashion industry...
Read MoreWeight Gain In Menopause
Many people wonder if weight gain in menopause is common....
Read MorePostpartum Diet Plan: Tips For Healthy Weight Loss
The postpartum period is a critical phase in a new...
Read MoreDoctor Explains Treatment For Postpartum Foot Pain
Postpartum foot pain is a common issue. It is experienced...
Read MoreExercises For Diastasis Recti
Diastasis recti in pregnancy is very common, and postpartum fitness...
Read MoreHow Many Lactation Cookies Should I Eat?
Many moms on their breastfeeding journey wonder, “How many lactation...
Read MoreHow Long Postpartum Bleeding Will Last
Are you wondering, how long postpartum bleeding will last after...
Read MorePostpartum Gifts For Mom: 6 Great Options
Postpartum is a tough time for most moms. You are...
Read MorePostpartum Sex Tips
In general, healthcare providers recommend waiting at least six weeks...
Read More5 Essential Breastfeeding Tips
Breastfeeding is very physically and emotionally challenging. In order to...
Read MoreMini Fridge For Breast Milk: Best Choices
Do you need a mini fridge for storing breast milk?...
Read MoreBreastfeeding For Birth Control
Using breastfeeding as birth control can be done but there...
Read MoreHow Often Should I Pump To Increase Milk Supply
The best way to increase breast milk supply fast is...
Read MorePostpartum Doula Contract Template For Post Birth
Postpartum doula services can be incredibly helpful both during the...
Read MoreIndian Vegan Recipes For Dinner: Cauliflower 65
This cauliflower Indian recipe is great for a quick and...
Read MoreVegan Restaurants In NYC 2022
There’s no better place to find a vegan restaurant than...
Read MoreVegan Pesto: Two Easy Recipes
This easy vegan pesto is a great option for people...
Read MoreBaked Eggplant Recipe: Vegetarian Or Vegan
This easy vegetarian baked eggplant dish can also easily be...
Read MoreHealthy Overnight Oats Recipe
Looking for a healthy overnight oats recipe? Well, you have...
Read MoreEasy PCOS Friendly Recipes For Nutritious Meals
Patients with Polycystic Ovary Syndrome often suffer from insulin resistance...
Read More